 Subcutaneous injections: Injecting at home
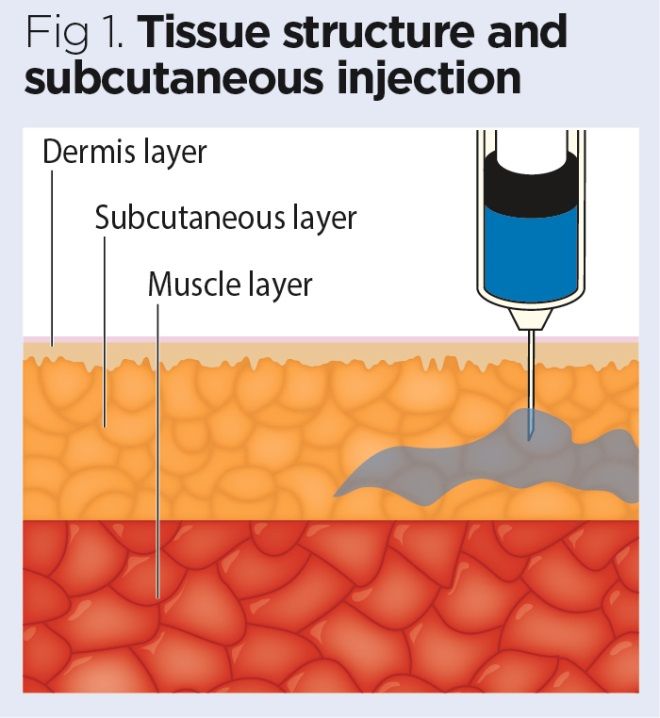
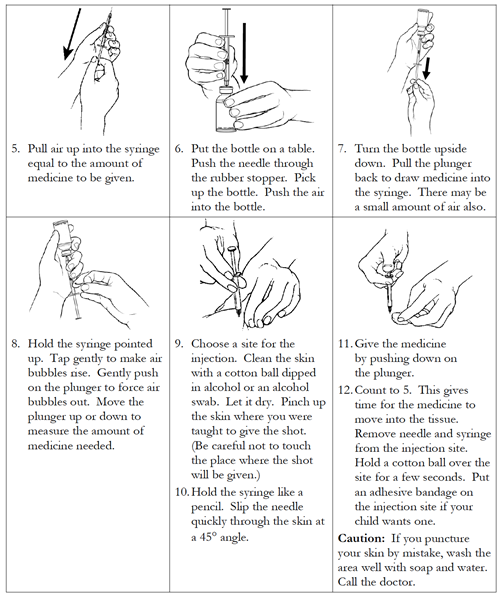
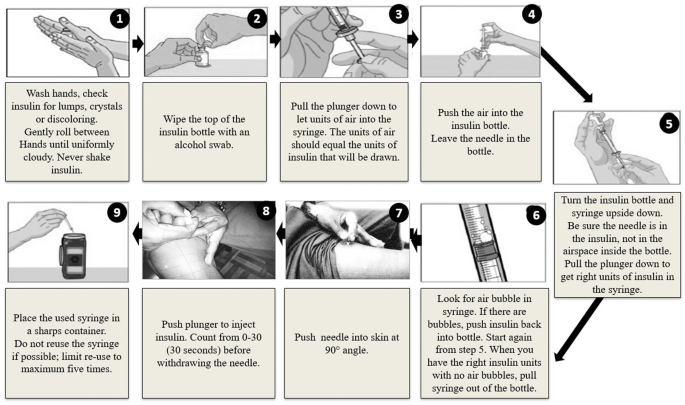
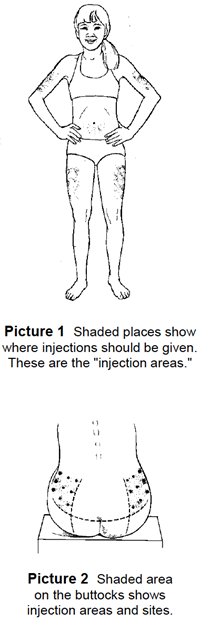
Subcutaneous injections: Injecting at homeChapter 1. Infection Control 2. Patient assessment character 3. Handling, Positioning and Transfer of Safe Patients 4. Care for the wounded 5. Oxygen therapy 6. Administration of Non-Pateral Medicines Chapter 7. Parental Medicines Administration Mechanism 8. Intravenous TherapyChapter 9. Monitoring of blood glucose Chapter 10. Tubes and accessories 7. Parental Medicines Administration 7.3 Intradermal and subcutaneous injections Intradermal injections (IDs) are injections administered in the dermis, just below the epidermis. The ID injection route has the longest absorption time of all parenteral routes. These types of injections are used for sensitivity tests, such as TB (see Figure 7.13), allergy and local anesthesia tests. The advantage of these tests is that body reaction is easy to visualize, and the degree of reaction can be evaluated. The most common sites are the inner surface of the forearm and the upper back, under the escapula. Choose a lesion-free injection site, rash, topos or scarring, which may alter the visual inspection of test results (Lynn, 2011). The equipment used for identification injections is a tuberculin syringe calibrated in tenths and hundredths of a milliliter, and a needle of 1/4 to 1/2 inch, 26 or 27 calibers. The dose of an identification injection is usually less than 0.5 ml. The management angle for an ID injection is 5 to 15 degrees. Once the identification injection is completed, a buckle (small blister) should appear under the skin. Checklist 56 describes the steps to administer an intradermal injection. List 56: Manage intradermal injection (ID) Disclaimer: Always review and follow your hospital policy regarding this specific skill. Security considerations: Steps Additional information 1. Prepare medicines or solution according to agency policy. Make sure all the medication is correctly identified. Verify medical orders, the Parenteral Medicine Therapy Manual (PDTM), and the MAR to validate the order and guidelines of the medication for the administration. The proper identification of the medication decreases the risk of involuntarily administering the wrong medication. The preparation of medications ensures patient safety with the administration of medicines. Compare medical orders and MAR Prepare medicines from a jar 2. ; collect supplies. Gather all supplies: medication syringe, non-sterile gloves, alcohol gauze and sterile gauze, Band-Aid (if necessary). Resource requirements 3. Enter and enter, explain the procedure and the medication, and allow the patient to have time to ask questions. Explaining rationality increases patient knowledge and reduces anxiety. 4. Close the door or pull the curtains of the night. This provides patient privacy. 5. Compare SEA to the patient bracelet and verify that this is the correct patient using two identifiers. This ensures the accuracy of the medication or solution and prevents errors. Two patient identifiers are patient name and date of birth. Compare MAR with the patient bracelet 6. Evaluate the patient for any contraindication to medications. Evaluation is a prerequisite for each given medication. 7. Select the right site for the administration. Assist the patient to the right position as necessary. The site should be free of injuries, rashes and topos. The selection of the right site allows accurate reading of the test site at the right time. Evaluate the site for the injection of ID 8. and apply non-sterile gloves. Gloves help prevent exposure to contaminants. Apply non-sterile gloves 9. Clean the site with an alcohol hysop or antiseptic hysop. Use a firm and circular motion. Allow the site to dry. Skin pathogens can be forced to tissue by needle. Allow the dry skin to prevent alcohol from entering the tissue, which can be irritating and uncomfortable. Clean injection site 10. Remove the needle from the cap by pulling it into a straight move. This decreases the risk of accidental needle injury. Remove the needle from the lid 11. Using non-dominant hand, spread the skin blanket over the injection site. The Taut skin provides an easy entry for the needle. Keep the skin blanket before injection 12. Hold the syringe in the dominant hand between the thumb and the ancestor, with the needle hinge up. This allows easy syringe handling. Bezel clamping needle 13. Keep the syringe at an angle of 5 to 15 degrees from the site. Place the almost flat needle against the patient's skin, attach it and insert the needle into the skin. Insert the needle only about 1/4 ing, with all the bevel under the skin. Maintaining the side of the hinge upwards allows the smooth perforation of the skin and the induction of the medication in the dermis. Identification injection 14. Once the syringe is in place, slowly inject the solution while looking at a small bleeding or wood. The presence of bleeding or bleeding indicates that the medication is in the dermis. Presence of a bleb (high white circle) 15. Remove the needle at the same angle as insertion, involve safety shield or needle guard, and discharge into a container of sharpeners. Do not massage the area after injection. Retreating at the same angle as insertion minimizes discomfort to the patient and tissue damage. The proper removal of needles prevents needle lesions. syringe discovered in sharpened containers Massage in the area can extend the solution to the underlying subcutaneous tissue. Skat gently with sterile gauze if the blood is present. 16. If the injection is a TB skin test, circulate the area around the injection site to allow easy identification of the site in three days. Circle drawing around the injection site 17. Descender the remaining supplies, remove gloves, and . This prevents the spread of microorganisms. Hand hygiene with ABHR 18. Document the procedure and conclusions according to the policy of the agencies. Appropriate documentation helps ensure patient safety. Document time, date, location and type of medication injected. 19. Evaluate the patient's response to injection within the appropriate time frame. The patient will have to be evaluated for therapeutic and adverse effects of the medication or solution. Data source: ATI, 2015a; Berman & Snyder, 2016; Brookside Associates, 2015a; Clayton, Stock, & Cooper, 2010; Perry et al., 2014 Checklist 56: Manage Intradermal Injection (ID)Steps Additional InformationThe preparation of medicines guarantees patient safety with the administration of medicines. Two patient identifiers are patient name and date of birth. Do not massage the area after injection. The proper removal of needles prevents needle lesions. Massage in the area can extend the solution to the underlying subcutaneous tissue. Skat gently with sterile gauze if the blood is present. Subcutaneous injection Subcutaneous injections (SC) are administered in the adipose tissue layer just below the epidermis and dermis. This tissue has few blood vessels, so the drugs administered by this route have a slow and sustained absorption rate. SC injection sites include the outer appearance of the upper arm, the abdomen (from below the costly margin to the ilic crest) within an inch of the belly button, previous aspects of the thighs, the upper back and the upper ventral gluteum area (Lynn, 2011) (see Figure 7.14). Choose a site free from skin lesions and bone prominences. The rotation of the site prevents the formation of lipohipertrophy or lipoatrophy in the skin. Physical exercise or the application of hot or cold compresses influences the drug absorption rate by altering local blood flow to tissues. Any condition that impairs blood flow to subcutaneous tissue contradicts the use of subcutaneous injections. Examples of subcutaneous drugs include insulin, opioids, heparin, epinefrine, and allergy medications (Perry et al., 2014). To administer a SC injection, a calibre of 25 to 30, from 3/8 to 5/8 ing. It uses needle. Some subcutaneous injections are prefilled with the attached syringe. Always confirm that the right size needle is appropriate for the patient before use. Subcutaneous injections are usually given at an angle of 45 to 90 degrees. The angle is based on the amount of subcutaneous tissue present. Generally, it gives shorter needles at an angle of 90 degrees and longer needles at an angle of 45 degrees (Lynn, 2011). SC injections do not need to be aspirated as the probability of injecting into a blood vessel is small. Generally, more than 1 ml of medication is not given subcutaneously, since the larger amounts can cause discomfort to the patient and cannot be properly absorbed (Lynn, 2011). There are different opinions about whether to pinch the skin during administration. Pricking is advised for the thinner patients in order to elevate the fatty tissue up and away from the underlying muscle and tissue. If the pinch is used, release the pinch when the needle is inserted to prevent injection into the compressed tissue. Please also note that raising or pinching the skin has been found to increase the risk of injury, as the needle can pierce the opposite side of the skin fold and enter the skin of the health worker (Black, 2013). The abdomen is the best location for an injection of SC if a patient has little peripheral SC tissue. If the patient is obese, use a needle that is long enough to insert through the tissue at the base of the skin fold (Perry et al., 2014). Insulin SC InjectionsInsulin is considered a high-risk medication, and special care should be taken to ensure that the correct amount of medication and insulin type is given at the right time. In addition, security checks related to a patient who receives insulin SC (Ellis & Parush, 2012) should be performed. Specific guidelines for the administration of insulin are listed in table 7.5 (see figure 7.15). Table 7.5 Guidelines for the administration of insulin SC Insulin Additional information Insulin is considered a high-risk medication. Special care should be taken to ensure the correct amount of medications and the type of insulin is given at the right time. It is highly recommended to always get insulin doses checked twice by another healthcare provider. Always follow the standard for drug preparation in your agency. Insulin is only given using an insulin syringe. Insulin is the only drug with its own type of syringe with an attached needle. Insulin is always ordered and administered in units, based on a blood sugar reading and a diabetic insulin protocol (or slide scale). Some hospitals have issued medical orders, and some hospitals have written orders. Insulin syringes may come in measurements of 30, 50 or 100 units. Always read carefully the increases (calibration). There are different types of insulin. There are fast, short, intermediate and long-acting insulins. For each type of insulin, it is important to know how insulin works and the initiation, peak and duration of insulin. Manage two different types of Insulin. If a patient is ordered two types of insulin, some insulins can be mixed in a syringe. Many insulins cannot be mixed together. Do not mezcle Lantus (Glargine) or Levemir (Determine). If you administer cloud insulin preparations (Humulin – N), gently roll the bottle between the palms of your hands to reopen the medication. Always draw short-acting insulin first, to prevent it from being contaminated with long action. If too much insulin is removed from the second syringe, discard the syringe and start again. Always check with the PDTM for the most current guidelines on insulin management. Insulin orders can change from day to day. Always make sure you follow the most current medical orders. He knows the rotary injection sites. The rotation of the injection site is no longer necessary as newer insulins have a lower risk of hypertrophy of the skin. Typically, a patient will choose an anatomical area (e.g., upper arm) and rotate the injection sites within that region to keep the constant absorption of insulin day by day. Insulin absorption rates vary from site to site. The abdomen absorbs the fastest, followed by the arms, thighs and buttocks. Know when to administer insulin. The time of insulin injections is critical to correct insulin management based on blood sugar levels and when the patient will eat. Knowing the peak action and the duration of insulin is essential for the proper management of insulin drugs. If insulin is given, it always ensures that the patient is not nausea, can eat, and that the food arrives before the insulin begins to work. Typically, quick or short-acting insulin is given 15 minutes before meals. Intermediate or prolonged insulin can be given twice a day, at breakfast and dinner. Measure blood sugar levels and food intake. Insulin injections are based on blood sugar values and when the patient will eat. The time for an insulin injection is critical to ensure that the patient receives insulin correctly. Use insulin injection pens. Injection pens are a new technology used by patients to inject insulin through syringe, needle and prefilled insulin cartridge. It is essential that patients be taught how to use injection feathers to understand technology. A mini-infusion pump is a battery-operated machine that offers medication in very small quantities to patients with controlled infusion times. The most common types of mini-infusion assemblies are insulin pumps or subcutaneous infusion devices. For more information on mini-infusion assemblies and volume-controlled assemblies, see section 7.8. Data source: Canadian Diabetes Association, 2013; Perry et al., 2014 InsulinInsulin Additional Information A mini-infusion pump is a battery-operated machine that offers medicines in very small quantities to patients with controlled infusion times. The most common types of mini-infusion assemblies are insulin pumps or subcutaneous infusion devices. For more information on mini-infusion assemblies and volume-controlled assemblies, see section 7.8. Heparin SC InjectionsHeparin is an anticoagulant used to reduce the risk of thrombosis formation by suppressing clot formation (Perry et al., 2014). Heparin is also considered a high-performance medication (ISMP, 2014). Specific guidelines are provided in table 7.6 to review before and after the administration of heparin. Table 7.6 Guidelines for the administration of heparin SC Heparin Additional information Heparin is considered a high-risk medication. Heparin is available in prefilled vials and syringes in a variety of concentrations. Due to the dangerous adverse effects of the medication, high-risk medication is considered. Always follow the policy of agencies regarding the preparation and administration of heparin. Rotate heparin injection sites. It is important to rotate heparin sites to avoid bruising in a place. To minimize bruises and pain associated with heparin injections, they can be given in the abdominal area at least 5 cm away from the abdomen button. He knows the risks associated with heparin. There are many risks associated with the administration of heparin, including bleeding, hematuria, hematomesis, bleeding gums and melena. Check the lab values. Review laboratory values (PTT and aPTT) before and after heparin administration. Use prepackaged heparin syringes. Many agencies use prepackaged heparin syringes. Always follow the standards for safe administration of medications when using prefilled syringes. Low molecular weight heparin (LMWH) is more effective in some patients. Evaluate the conditions of patients before administration. Some conditions increase the risk of bleeding (swelling), such as recent delivery, severe diabetes, severe kidney and liver disease, severe traumas, cerebral or aortic aneurysm, strokes (CVA), blood discrases and severe hypotension. Evaluate medicines before administration. Free-selling herbal medicines (OTC), such as garlic, ginger and horse chestnut, can interact with heparin. Additional medications that may interact include Aspirin, NSAIDS, cephalosporins, anti-thyroid agents, thrombolytics, and proven. Data source: Clayton et al., 2010; Ogston-Tuck, 2014b; Perry et al., 2014 HeparinHeparin Additional InformationChecklist 57 provides the steps to complete a subcutaneous injection. List 57: Manage a Subcutaneous Injection Disclaimer: Always review and follow your hospital policy regarding this specific skill. Security considerations: Steps Additional information 1. Prepare medicines or solution according to agency policy. Always compare medical orders with the MAR. The preparation of medications ensures patient safety with the administration of medicines. Prepare medicines 2. ; collect supplies. You will need medication syringe, non-sterile gloves, alcohol crab and sterile gauze, Band-Aid. 3. Get in the room and sit down. Identify the patient using two acceptable identifiers, explain the procedure and the medication, and allow the patient to have time to ask questions. Explaining rationality increases patient knowledge and reduces anxiety. 4. Close the door or pull the curtains of the night. This provides patient privacy. 5. Compare SEA to the patient bracelet and verify that this is the correct patient using two identifiers. This ensures the accuracy of the medication or solution and prevents errors. Compare MAR with the patient bracelet 6. Evaluate the patient for any contraindication for medications. Evaluation is a prerequisite for the administration of medicines. 7. Put on unsterile gloves. Gloves help prevent exposure to contaminants. Apply non-sterile gloves 8. Select the right site for the administration. Assist the patient to the right position as necessary. The site should be free of injuries, rashes and topos. Choosing the right site allows an accurate reading of the test site at the right time. SC injection site (inside from the upper arm) 9. Clean the site with an alcohol hysop or antiseptic hysop. Use a firm and circular motion. Allow the site to dry. Skin pathogens can be forced to tissue by needle. Allow the dry skin to prevent alcohol from entering the tissue, which can be irritating and uncomfortable. Clean site with alcohol cano 10. Remove the needle cap with the non-dominant hand, pull it directly. This technique decreases the risk of an accidental needle injury. 11. Grab or pinch the area surrounding the injection site, or spread the skin blanket on the site. The decision to create a fold of the skin is based on the assessment of the patient's nurse and the length of the needle used. Pricking is advised for thinner patients. Select the SC site (in reverse of the upper arm) 12. Hold the syringe in the dominant hand between the thumb and the ancestor. Insert the needle quickly at an angle of 45 to 90 degrees. The insertion quickly causes less pain to the patient. Subcutaneous tissue is abundant in people well nourished and well hydrated. For patients with little subcutaneous tissue, it is best to insert the needle at a 45-degree angle. 13. After the needle is in place, release the tissue. Move your non-dominant hand to hold firm and lower the end of the needle. With the dominant hand, inject the medication at a speed of 10 seconds per ml. Avoid moving the syringe. Keeping the needle stable helps keep the needle in place. SC injection Injectable medicine 14. Remove the needle quickly at the same angle it was inserted, while supporting the surrounding tissue with the non-dominant hand. Retiring at the same angle prevents tissue damage and increased pain at the injection site. 15. Using a sterile gauze, apply a soft pressure on the site after removing the needle. Don't massage the site. Massage is not necessary and can damage the underlying tissue. Massage after a heparin injection can contribute to the formation of a hematoma. 16. Don't recapture the needle. Apply the safety shield or needle protector on the needle and discard in a sharp container. Security shields and needle protectors help prevent accidental needle injuries. SC needle with safety shield syringe discovered in sharpened containers 17. Provision of supplies; remove gloves and . This reduces the risk of infection and the spread of microorganisms. Hand hygiene with ABHR 18. Procedure of documents and conclusions according to agency policy. Timely documentation ensures patient safety. 19. Evaluate the patient's response to the medication. It is important to evaluate the therapeutic effect of the medication and to evaluate the adverse effects. Data source: ATI, 2015b; Berman & Snyder, 2016; Brookside Associates, 2015b; Clayton et al., 2010; National Institute of Health Clinical Center, 2015; Ogston-Tuck, 2014b; Perry et al., 2014 Checklist 57: Manage Subcutaneous InjectionSteps Additional Information Critical Thinking ExercisesLicense by British Columbia Institute of Technology (BCIT) is licensed under one, except where otherwise indicated. Share this book
EMI Filter DesignEMI Filter Design, Third EditionDevelopment of practical nursing skills

A nurse preparing a section of skin for an injection is an example of ______. - Brainly.com
Intramuscular injections: Injecting at home
Intramuscular Injection: Definition and Patient Education
Intramuscular Injection: Definition and Patient Education
Intramuscular Injection: Definition and Patient Education
Intramuscular Injection: Definition and Patient Education
Intramuscular Injection: Definition and Patient Education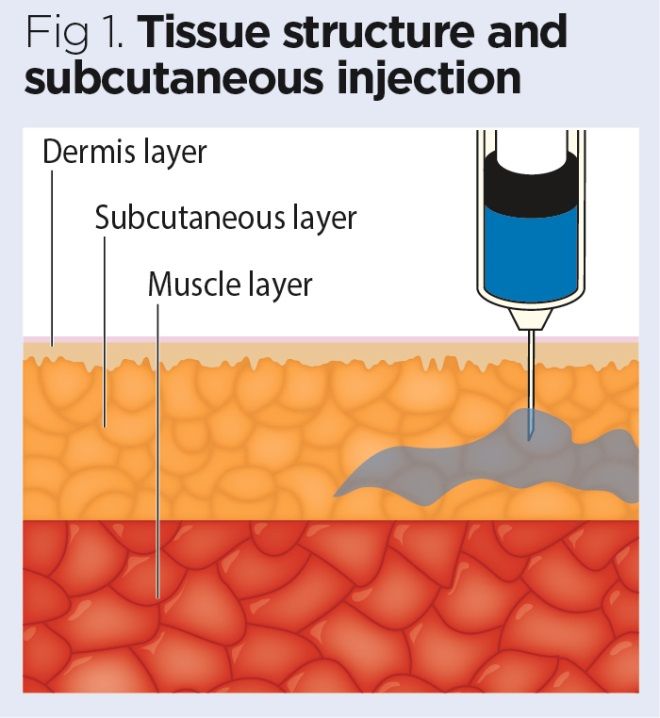
Administering Drugs via a Subcutaneous Injection | Nursing Times
Are blown veins harmful? Symptoms, causes, and treatment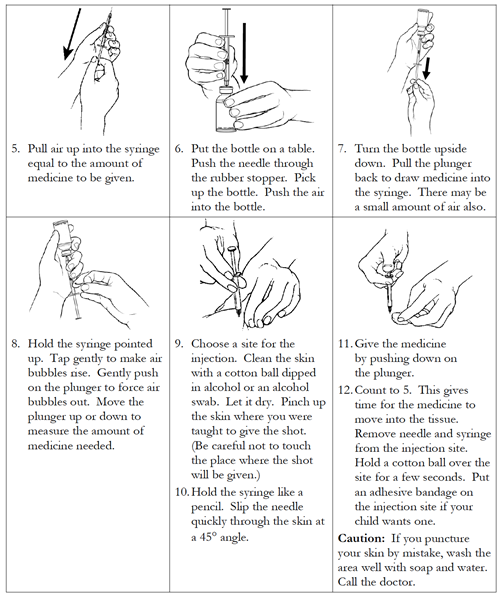
Injections Subcutaneous
NYU Microbiology Ch. 9 & 22 Flashcards | Quizlet
Subcutaneous Injection: Definition and Patient Education
Administering Drugs via a Subcutaneous Injection | Nursing Times/nurse-holding-a-syringe-for-the-injection-giving-patient-vaccine-in-hospital--health-care-concept-1144801757-6876c19867a8477c8596d385b53aef58.jpg)
Z Track Method of Injection: Procedure and Side Effects
Z-Track Injection | Definition and Patient Education
Pfizer CEO says it's 'radical' to suggest pharma should forgo profits on COVID-19 vaccine: report | FiercePharma
Subcutaneous Injection: Definition and Patient Education
MCQs for Entrance Test for BN, MN, MSN Nursing by RS MEHTA
Intramuscular injections: Injecting at home
Subcutaneous Injection: Definition and Patient Education
Specimen Collection & Procedures: A Nurse's Guide
EADSG Guidelines: Insulin Storage and Optimisation of Injection Technique in Diabetes Management | SpringerLink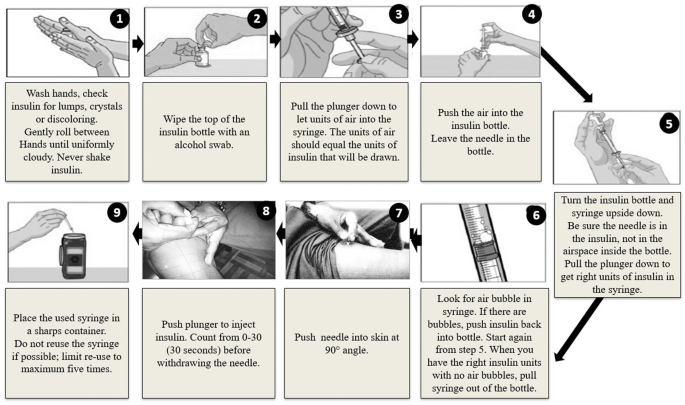
EADSG Guidelines: Insulin Storage and Optimisation of Injection Technique in Diabetes Management | SpringerLink
Administering Drugs via a Subcutaneous Injection | Nursing Times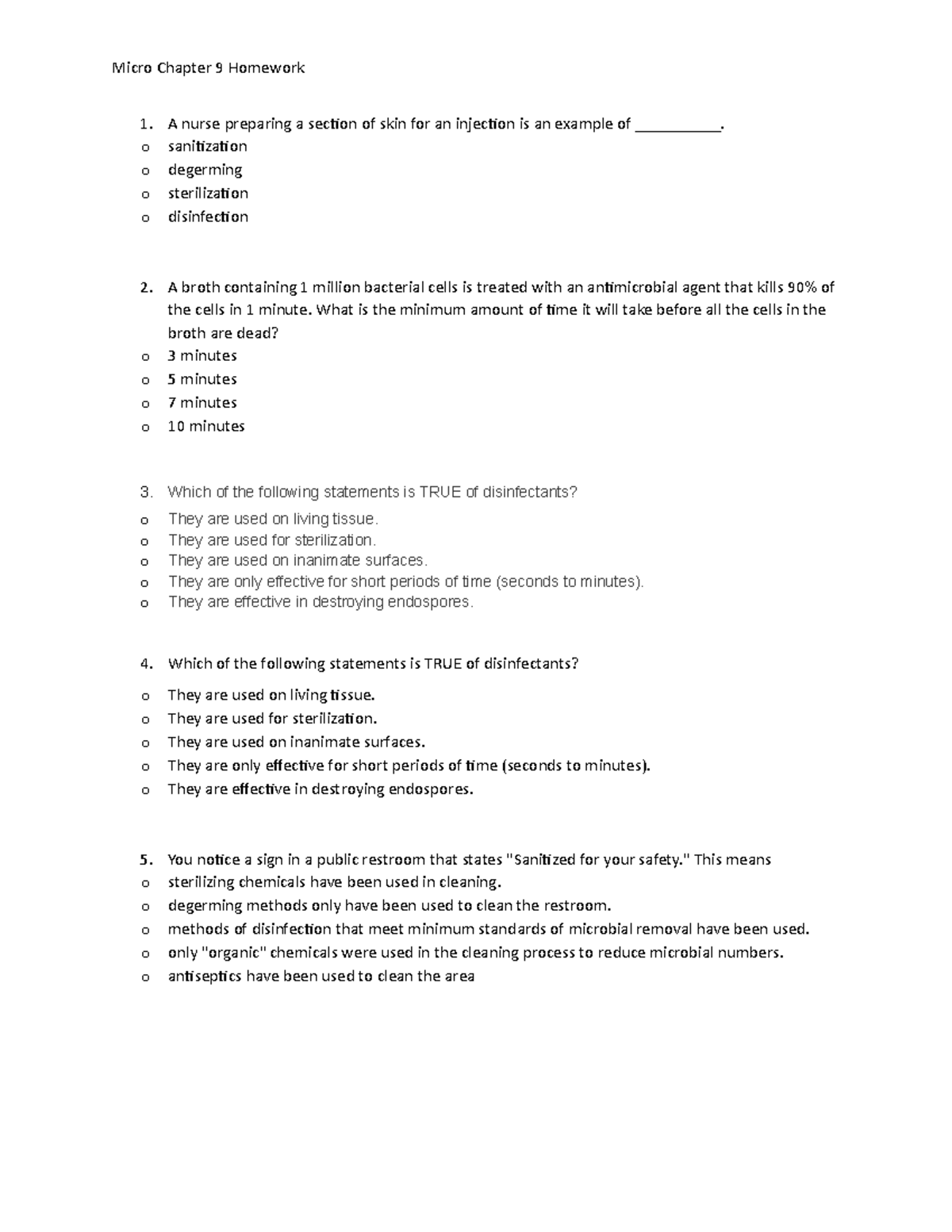
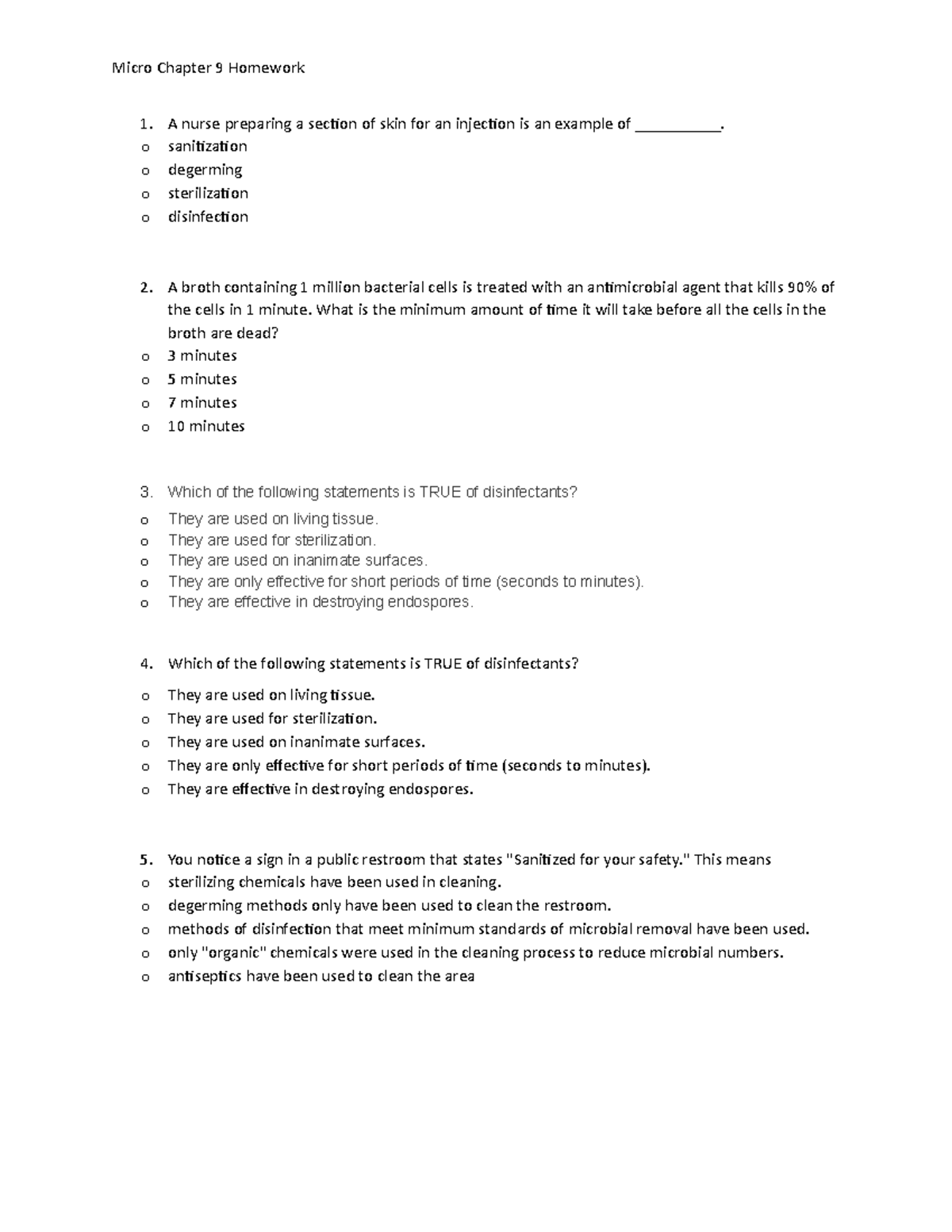
Micro chapter 9 homework - TAMUCC - StuDocu
Intramuscular Injection: Definition and Patient Education
The alcohol swab before the needle: A point of debate - Hospital News
TACTILE TOUCH IN INTENSIVE CARE Nurses' preparation, patients' experiences and the effect on stress parameters
Comprehensive Overview of Nursing and Interdisciplinary Care of the Acute Ischemic Stroke Patient | Stroke
Skin Preparation for Injections: A Review of Clinical Effectiveness, Cost-Effectiveness and Guidelines - NCBI Bookshelf
The First Shot: Inside the Covid Vaccine Fast Track | WIRED
Intramuscular injections: Injecting at home
Gaining Insite Harm Reduction in Nursing Practice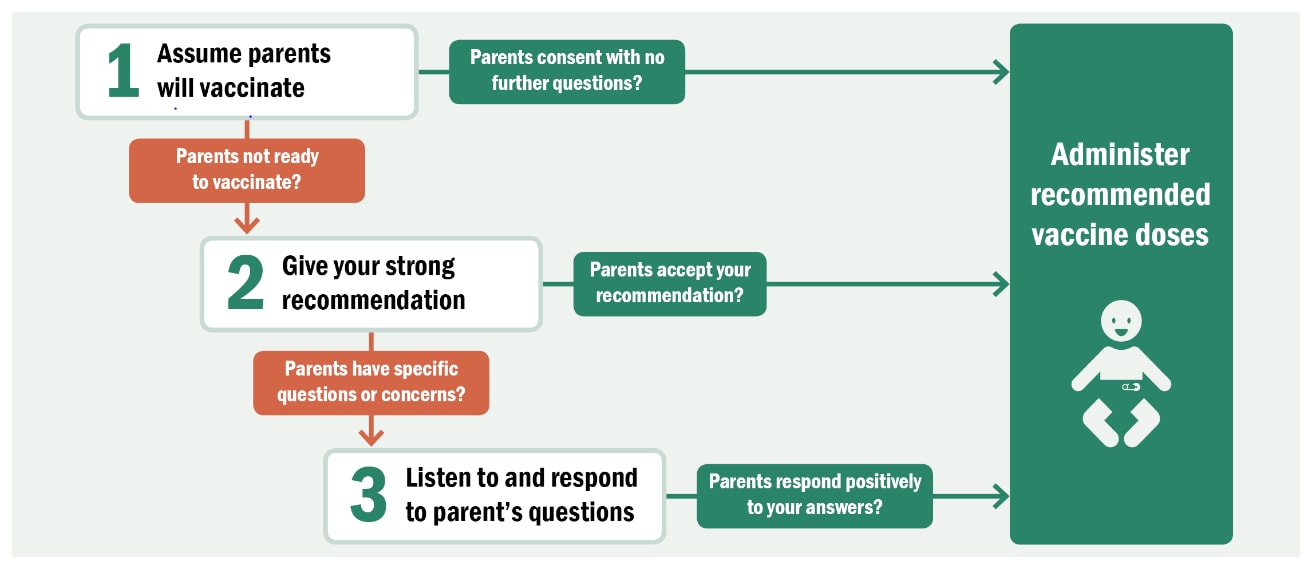
Pinkbook | Vaccine Administration | Epidemiology of VPDs | CDC
Blog | COVID-19
Subcutaneous Injection: Definition and Patient Education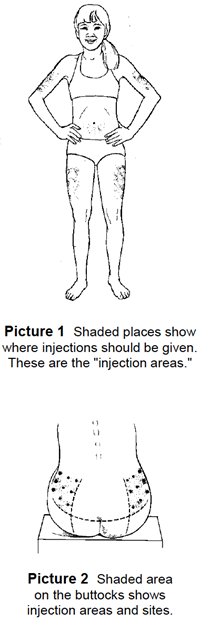
Injections Subcutaneous
Subcutaneous Injection: Definition and Patient Education
Package leaflet: Information for the user HUMULIN® S (Soluble) 100 IU/ml solution for injection in vial (Insulin human) Read al
 Subcutaneous injections: Injecting at home
Subcutaneous injections: Injecting at home










/nurse-holding-a-syringe-for-the-injection-giving-patient-vaccine-in-hospital--health-care-concept-1144801757-6876c19867a8477c8596d385b53aef58.jpg)
















Posting Komentar untuk "a nurse preparing a section of skin for an injection is an example of ."